A melanoma diagnosis can be a confusing and traumatic time for you and your loved ones, so we want to provide you with knowledge and support.
How is Melanoma Diagnosed?
Initial diagnosis
Most melanoma diagnoses start with a suspicious looking spot on the skin. If you see a strange new mole on your skin or an old mole that’s started changing be sure to see your doctor right away, because an early diagnosis makes a big difference to your outcome. Please refer to the following pages for more information:
Your doctor will do a physical examination to check all parts of your skin including your hands and feet, inside your mouth and nose and your scalp. They might use a magnifying instrument called a dermatoscope to refine their diagnosis. If they find something they’re uncertain about you might be referred to a dermatologist. If they find something suspicious they’ll recommend you have a biopsy.
A biopsy is the removal of a tissue sample from the suspicious area so that it can be sent to a pathologist for examination.
Biopsy
A biopsy can determine whether there are melanoma cells present in a suspicious looking spot or lump. Once a biopsy has been taken, the sample will be sent to a pathologist for examination.
Common biopsy procedures include:
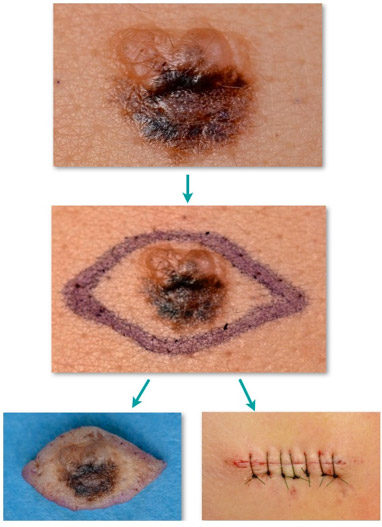
- Excision biopsy – where a scalpel is used to remove the entire affected area and often some healthy tissue for examination. It is a simple procedure that can be done by your GP, dermatologist or a surgeon under local anaesthetic. The sample will be sent to pathology.
- Punch biopsy – which involves the removal of a circular area of skin with an instrument known as a punch
- Shave biopsy – where a superficial area of the lesion is taken off, often with a razor-type blade
- Fine needle biopsy – where a needle similar to that used for blood collection is used to capture a sample of cells
Pathology
Once a biopsy has been taken, the sample will be sent to a pathologist for examination. A pathologist is a specialist doctor who examines tissue under a microscope to detect diseased cells. The pathology results will be ready in about a week. You will likely have a follow-up appointment for you and your doctor to discuss the results and further procedures or treatment recommendations.
Reading a pathology report
Terms commonly used in pathology reports are explained below. If you have further questions, talk to your doctor.
Types of melanoma
There are different types of melanoma and your pathology report will outline how your melanoma is classified.
- Superficial spreading melanoma – this is the most common type of melanoma making up about 50% of all melanomas diagnosed. This melanoma usually appears as a dark spot with irregular borders that spreads across the skin.
- Nodular melanoma – this is one of the most rapidly growing types of melanoma. It appears as a raised lump or ‘nodule’ and can be brown, black, pink or red in colouring, or have no colour at all. About 15% of all melanomas are nodular.
- Acral lentiginous melanoma – this is a rare type of melanoma on the palms of hands, soles of the feet or under the nails (subungual). It accounts for about 3% of all melanomas.
- Desmoplastic melanoma – a rarer form of melanoma. It usually appears as a spot that may look like a scar in texture.
- Naevoid melanoma – a rarer form of melanoma. Challenging to diagnose because it looks a lot like a benign skin mole. It can be any color, including brown, black, blue, or red, and tends to be dome-shaped.
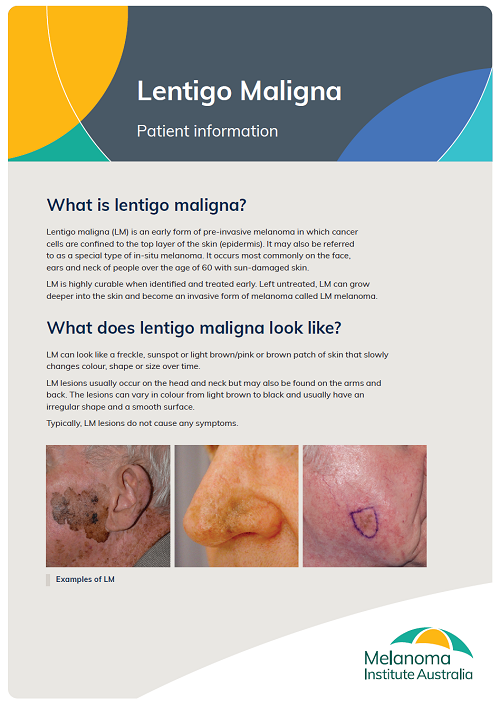
- Lentigo maligna melanoma – this usually begins as large freckles. They are commonly found in older people, often in areas that have received a lot of sun exposure such as the face, head, neck and upper body. This type of melanoma makes up 10% of all melanomas. Download brochure by clicking on cover image.
- Mucosal melanoma – melanoma found in the lining of the respiratory, digestive, and reproductive tracts. Download brochure by clicking on cover image.
- Uveal (ocular) melanoma – melanoma found in the eye. Download brochure by clicking on cover image.
Breslow thickness
This is the depth of your melanoma in millimetres and is used along with other features to stage the melanoma. Thinner melanomas have a better prognosis.
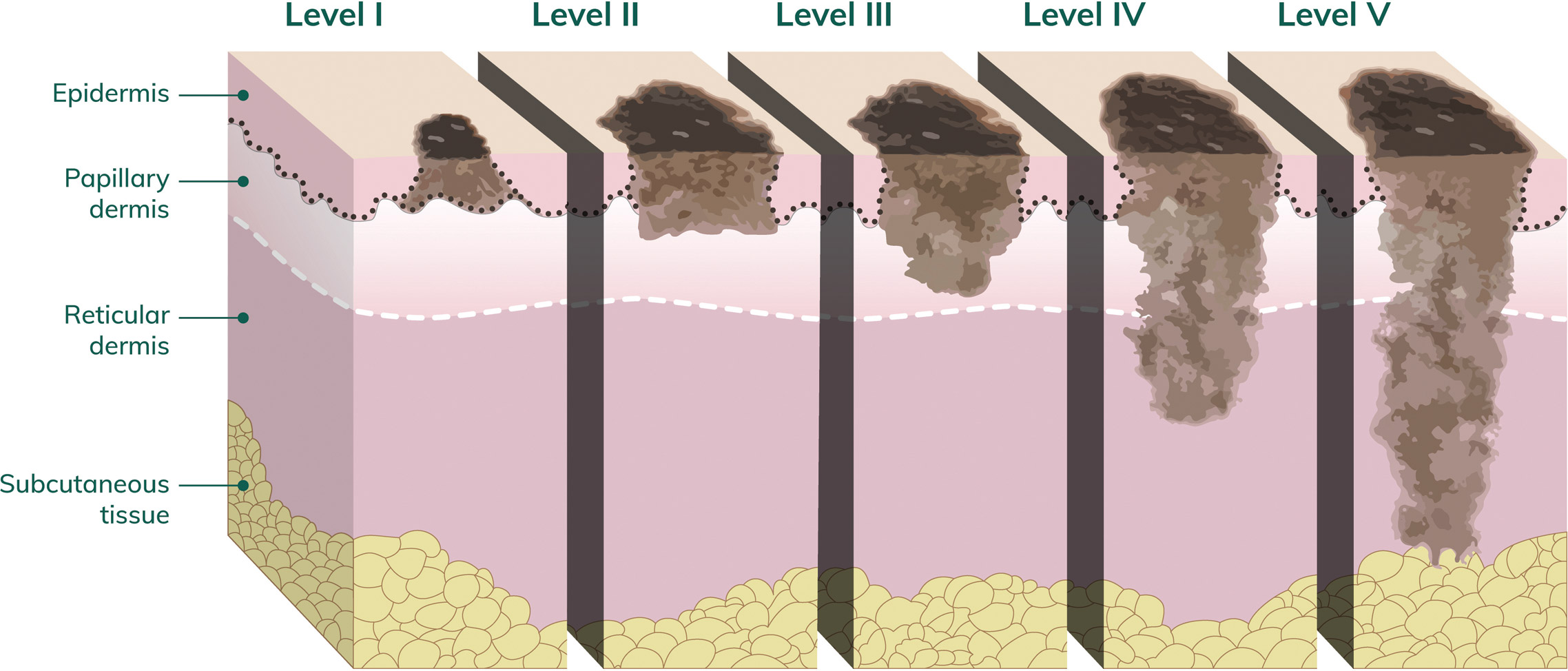
Clark level
This is a number that ranges from 1–5 (written in Roman numerals I–V) to describe how deeply the cancer has penetrated the skin. Clark level 5 (V) is the deepest level of invasion.
Ulceration
Ulceration is the breakdown of the top layer of skin over the melanoma. The presence or absence of ulceration is used to help determine the stage of melanoma. The presence of ulceration indicates a more rapidly growing melanoma.
Dermal mitoses
This describes how quickly the melanoma cells are dividing. Higher mitotic rates (e.g. greater than 5 per mm²) indicate faster growing melanoma and are associated with a worse prognosis.
Surgical margin
Your pathology report may describe the presence or absence of melanoma cells at the edges or deepest part of the sample (surgical margins). If these margins are positive (melanoma cells are present) more surgery may be needed.
Lymph node pathology report
If you have had a sentinel node biopsy, or you have had lymph nodes removed during surgery, the pathology report you receive after these procedures will record information about the number of nodes retrieved, the number of nodes containing melanoma and whether the melanoma has breached the node (called extra-nodal spread). The greater the number of lymph nodes containing melanoma, the poorer the prognosis. Extra-nodal spread is also associated with a poorer prognosis.
Stages of melanoma
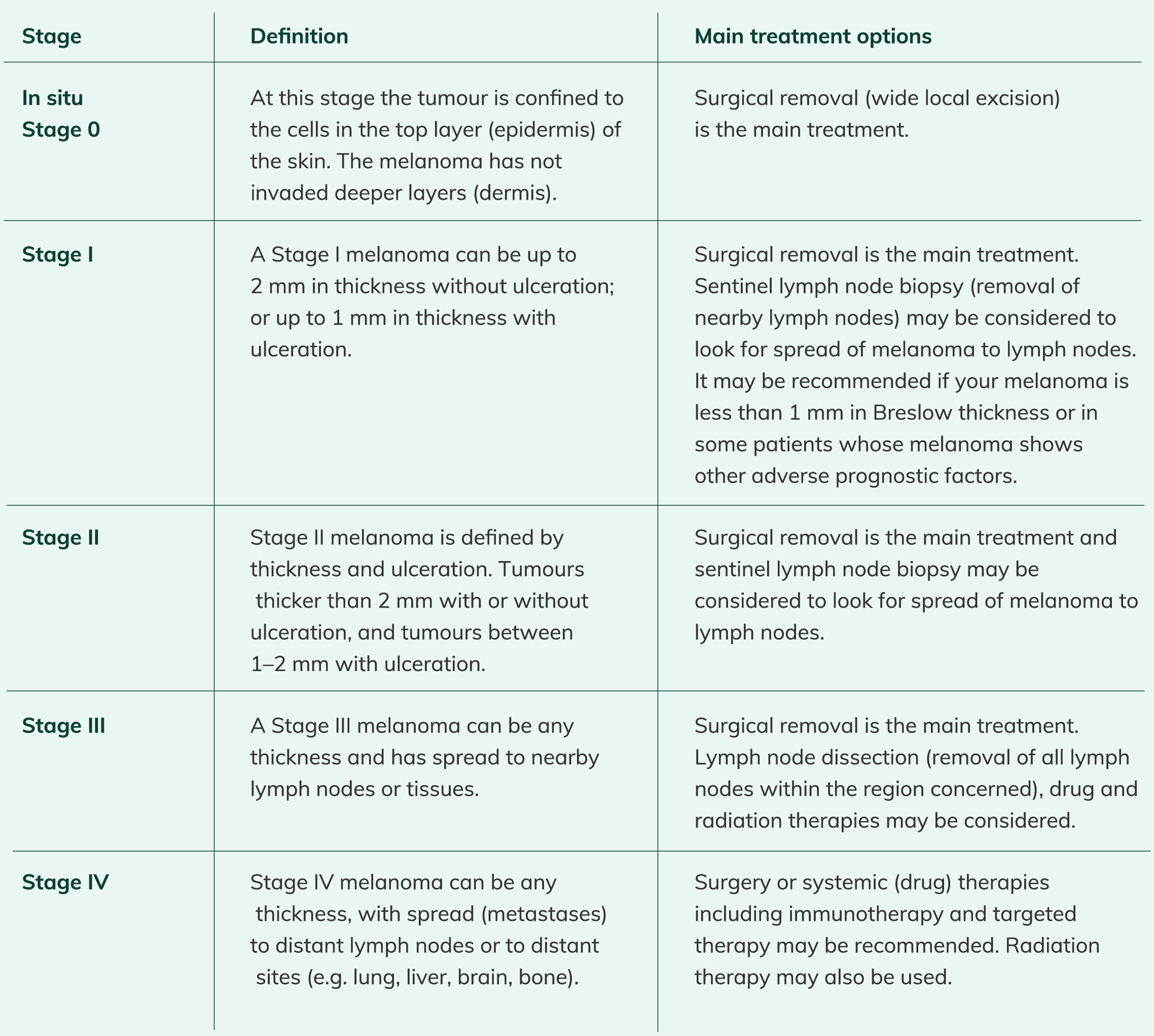
Staging a melanoma provides a description of its size and whether it has spread to other parts of the body. The stage of your melanoma helps to guide your treatment.
There are three ways to stage a melanoma, and all patients will undergo at least two of these:
- Microstaging – A histopathologist looks closely at tissue under a microscope using special dyes and techniques to look for specific features that will help inform how far the disease has spread.
- Clinical staging – The lymph node groups that relate to the location of the melanoma are carefully examined to for any evidence of spread, usually seen by enlarged lymph nodes.
- Staging after investigation – This involves the use of imaging scans to see inside the body, including CT, MRI, and PET scans.
Melanoma is staged as O, I, II, III or IV. It can also have a substage (a-d). The following table outlines the different
stages of melanoma, and relevant treatment pathways:
Patient information
To support you on your melanoma journey we have created guides for each stage of melanoma. Download our Patient Information Guides.
For more information about your how melanoma is diagnosed and staged see our Pathology and Staging leaflet.